DIAGNOSIS
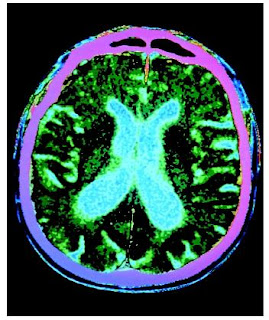
Cardiology diagnosis was systole, secondary to enhanced vagary tone form the left temporal lobe-onset seizures.
TREATMENT and Outcome
The patient underwent implantation of a dual-chamber pacemaker. Since then, she has continued to have both type of seizures but has not fallen to the ground in association with the second type. She has elected to defer epilepsy surgery at this time.
Discussion
Ictal-indeed changes in heart rate and rhythm are among the many possible autonomic manifestations of seizures. Sinus tachycardia is the most frequent disturbance of cardiac rate that accompanies seizures.In one series of consecutive patients with temporal lobe seizures, ictal tachycardia was associated with left-sided seizure onset onset in four patients and right temporal lobe onset in eight patients.
Bradyarrhythmias, including bradycardia, sinus arrest, atrioventricular block, and a systole occurs less frequently than tachyarrhythmias. In some patients with ictal-indude bradyarrthmia, less of consciousness may be due to sync Ope and not to the seizure. In this patient, a chance in heart rate, although it is likely that falls were associated with cardiac asystole.
Cardiology diagnosis was systole, secondary to enhanced vagary tone form the left temporal lobe-onset seizures.
TREATMENT and Outcome
The patient underwent implantation of a dual-chamber pacemaker. Since then, she has continued to have both type of seizures but has not fallen to the ground in association with the second type. She has elected to defer epilepsy surgery at this time.
Discussion
Ictal-indeed changes in heart rate and rhythm are among the many possible autonomic manifestations of seizures. Sinus tachycardia is the most frequent disturbance of cardiac rate that accompanies seizures.In one series of consecutive patients with temporal lobe seizures, ictal tachycardia was associated with left-sided seizure onset onset in four patients and right temporal lobe onset in eight patients.
Bradyarrhythmias, including bradycardia, sinus arrest, atrioventricular block, and a systole occurs less frequently than tachyarrhythmias. In some patients with ictal-indude bradyarrthmia, less of consciousness may be due to sync Ope and not to the seizure. In this patient, a chance in heart rate, although it is likely that falls were associated with cardiac asystole.
Recognition of the cardiovascular manifestation of seizures requires a high index of suspicion. This case illustrates that patients with abrupt falls following the onset of typical complex partial seizures should be evaluated for possible ictal-related cardiac conduction disturbances with simultaneous ECG and EEG monitoring.
In this particular case the patient had medically refractory simple partial and complex partial seizures. The latter was often associated with abrupt falling to the ground if she was standing during the seizure. Over the years, it was assumed that the patient's falls to the ground were a direct effect of the seizures on the strength and tone of her lower extremities. Only when she underwent ictal EEG monitoring did it becomes apparent that there was an alternative explanation-cardiac asystole. This is supported by the fact that she has not fallen since implantation of a cardiac pacemaker even though she continues to have the other typical manifestation of her seizures. Independent of her seizures, the patient had no other clinical evidence of cardiac arrhythmia's.
References
1. Schachter SC. Autonomic epilepsy. Se min Neurol 1995;15;158-66
2. Devin sky O, Price BH, Cohen SI. Cardiac manifesting of complex partial seizures. Am J Med 1986;56;443-46.
In this particular case the patient had medically refractory simple partial and complex partial seizures. The latter was often associated with abrupt falling to the ground if she was standing during the seizure. Over the years, it was assumed that the patient's falls to the ground were a direct effect of the seizures on the strength and tone of her lower extremities. Only when she underwent ictal EEG monitoring did it becomes apparent that there was an alternative explanation-cardiac asystole. This is supported by the fact that she has not fallen since implantation of a cardiac pacemaker even though she continues to have the other typical manifestation of her seizures. Independent of her seizures, the patient had no other clinical evidence of cardiac arrhythmia's.
References
1. Schachter SC. Autonomic epilepsy. Se min Neurol 1995;15;158-66
2. Devin sky O, Price BH, Cohen SI. Cardiac manifesting of complex partial seizures. Am J Med 1986;56;443-46.